If you’ve ever had a claim rejected because of a “non-specific” diagnosis code, you know how frustrating hyperlipidemia coding can be.
The ICD-10 codes for this condition seem simple at first glance—but the moment you add “mixed,” “familial,” or “secondary” into the mix, the game changes.
This guide breaks everything down for you — from choosing the correct ICD-10 codes to understanding payer expectations, documentation, and billing tips to avoid denials.
What is Hyperlipidemia?
Hyperlipidemia refers to abnormally high levels of lipids (fats) in the blood. These include cholesterol and triglycerides. It’s one of the most common conditions in adults, often linked with obesity, diabetes, and heart disease.
In simple terms: too much fat in your blood = higher risk of clogged arteries = higher risk of heart attack or stroke.
Clinically, hyperlipidemia is classified into:
- Primary (genetic) – caused by inherited lipid metabolism disorders.
- Secondary (acquired) – caused by lifestyle factors or other diseases like diabetes, hypothyroidism, or chronic kidney disease.
ICD-10 Codes for Hyperlipidemia
In ICD-10-CM, hyperlipidemia codes fall under the category E78 – Disorders of lipoprotein metabolism and other lipidemias.
Here’s the breakdown:
| ICD-10 Code | Description |
| E78.0 | Pure hypercholesterolemia |
| E78.00 | Pure hypercholesterolemia, unspecified |
| E78.01 | Familial hypercholesterolemia |
| E78.1 | Pure hyperglyceridemia |
| E78.2 | Mixed hyperlipidemia |
| E78.3 | Hyperchylomicronemia |
| E78.4 | Other hyperlipidemia |
| E78.49 | Other specified hyperlipidemia |
| E78.5 | Hyperlipidemia, unspecified |
| E78.6 | Lipoprotein deficiency |
| E78.9 | Disorder of lipoprotein metabolism, unspecified |
Most commonly used:
- E78.5 – Hyperlipidemia, unspecified
- E78.2 – Mixed hyperlipidemia
However, “unspecified” should be a last resort. Payers increasingly deny claims using E78.5 unless documentation clearly supports why no specific subtype could be identified.
| Common Coding Scenarios Mixed Hyperlipidemia ICD-10: E78.2 Use this when both cholesterol and triglyceride levels are elevated. This is the most frequently reported form and is often tied to metabolic syndrome. Example: A 55-year-old male presents with elevated LDL and triglycerides. No genetic disorder is suspected. → Code: E78.2 Familial Hypercholesterolemia ICD-10: E78.01 Use when there’s a genetic cause (family history and lab confirmation). Example: A 32-year-old with high LDL since childhood, with a strong family history of early heart disease. → Code: E78.01 Pure Hypercholesterolemia (Non-Familial) ICD-10: E78.00 Use when only cholesterol is elevated, but no familial or mixed cause. Example: Cholesterol 280 mg/dL, normal triglycerides. No family history. → Code: E78.00 Secondary Hyperlipidemia Secondary hyperlipidemia results from another condition, like diabetes or hypothyroidism. In such cases, code both the underlying cause and the hyperlipidemia. Example: Patient with Type 2 diabetes and elevated lipids. → Codes: E11.69 (Type 2 diabetes with other specified complication) E78.5 (Hyperlipidemia, unspecified) |
Documentation Guidelines for Hyperlipidemia ICD-10
Accurate documentation is the backbone of correct ICD-10 coding. Providers should note:
- Type of hyperlipidemia (mixed, pure, familial, secondary)
- Lab values (LDL, HDL, triglycerides)
- Underlying or contributing diseases
- Family history is relevant
- Current treatment (statins, lifestyle modification, etc.)
Example of good documentation:
“Patient presents with mixed hyperlipidemia (E78.2). LDL: 190 mg/dL, triglycerides: 230 mg/dL. No familial component identified. Plan: Continue atorvastatin 40 mg daily.”
Coding with Comorbidities
Hyperlipidemia rarely stands alone. It’s often linked with conditions like:
- Diabetes mellitus (E11.-)
- Hypertension (I10)
- Obesity (E66.-)
- Coronary artery disease (I25.1)
Always code these comorbidities when relevant, as they affect reimbursement and risk adjustment scores (HCC coding).
For example:
A diabetic patient with hyperlipidemia and hypertension
→ Codes: E11.69, E78.2, I10
Billing and Reimbursement Guidelines
Here’s how to ensure you get adequately paid for hyperlipidemia-related services:
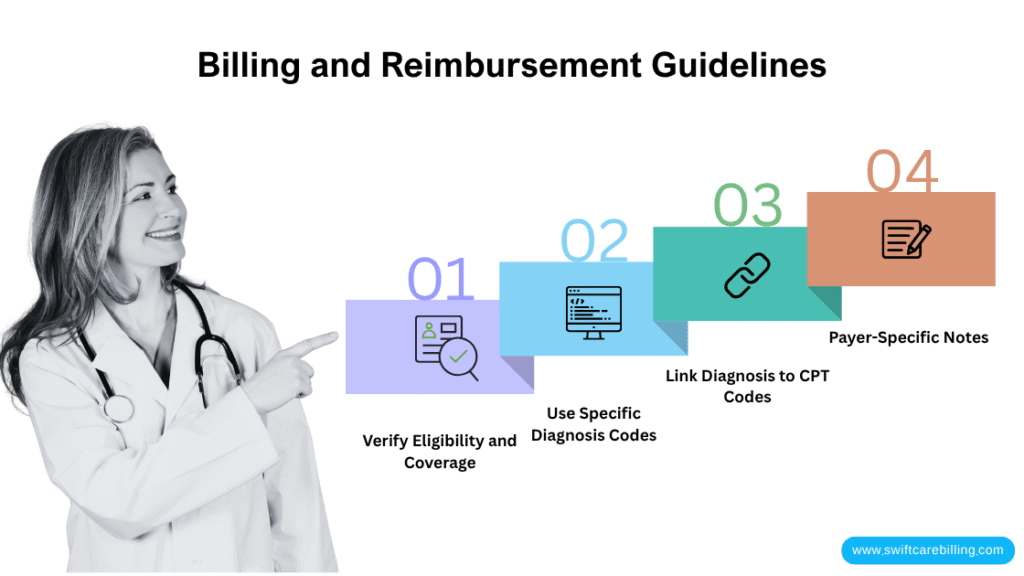
Verify Eligibility and Coverage
Check insurance eligibility before testing or treatment. Some payers require prior authorization for lipid panels beyond annual wellness visits.
Use Specific Diagnosis Codes
Avoid “E78.5” unless you have no specific findings. Payers prefer “E78.2” (mixed) or “E78.00” (pure).
Link Diagnosis to CPT Codes
When billing lipid panels or related visits, diagnosis codes must justify the medical necessity.
Common CPT Codes:
| Procedure | CPT Code | Common Pairing ICD-10 |
| Lipid panel | 80061 | E78.2, E78.5 |
| Office visit (established) | 99213–99215 | E78.x |
| New patient visit | 99203–99205 | E78.x |
| Counseling for diet/lifestyle | 99401–99404 | E78.x |
Payer-Specific Notes
- Medicare: Covers lipid screening once every 5 years for asymptomatic adults, but diagnostic testing can be done as needed with documented risk.
- Commercial plans: May allow annual lipid panels if justified by comorbidities.
- Medicaid: Coverage depends on state rules—always confirm prior authorization requirements.
Hyperlipidemia Coding and Billing Errors and How to Prevent Them
Even though hyperlipidemia seems simple to code, it’s one of the quiet money-leakers in internal medicine billing.
Why? Because payers love to deny lipid-related claims that lack specificity, proper linkage, or clear documentation.
Let’s walk through the most common denial causes tied to hyperlipidemia ICD-10 codes — and how to fix (and prevent) them.
Using “Unspecified” Code (E78.5) Without Supporting Detail
Many providers still default to E78.5 (Hyperlipidemia, unspecified) for every lipid-related visit.
It’s quick, but payers are cracking down on unspecified codes—primarily Medicare and Blue Cross plans.
If your documentation doesn’t justify why the condition is “unspecified,” you’ll likely see:
“Denial Reason: Non-specific or invalid diagnosis code for the date of service.”
How to Prevent It:
Always specify the type:
- E78.00 → Pure hypercholesterolemia
- E78.2 → Mixed hyperlipidemia
- E78.01 → Familial hypercholesterolemia
If you genuinely can’t determine the type (no labs yet, first-time visit), document why it’s unspecified:
“Initial lipid results pending; provisional diagnosis of hyperlipidemia, unspecified (E78.5).”
Follow up once the results are back and update the code.
Electronic health record (EHR) systems often let you “update diagnosis on resubmission.” Use that feature.
CPT and ICD-10 Mismatch
This happens when the billed service (CPT code) doesn’t “match” the diagnosis code (ICD-10) under payer logic.
Example: you billed a lipid panel (80061) but attached I-10 (Hypertension) as the only diagnosis.
To the payer, that looks like:
“Why are you ordering cholesterol testing for a blood pressure diagnosis?”
Common Problem Pairs:
| CPT | Mistaken Diagnosis | Correct ICD-10 |
| 80061 (Lipid panel) | I10 (Hypertension) | E78.2 or E78.5 |
| 99213 (Office visit) | R79.89 (Abnormal findings) | E78.2, E78.01, etc. |
How to Prevent It:
- Always link each CPT to its correct ICD-10 justification.
- In your EHR, double-check the diagnosis linking column—it’s easy to miss when multiple diagnoses are listed.
- Use claim scrubbing tools to catch mismatches before submission.
Missing Documentation or Lab Values
Payers often deny lipid-related claims due to “lack of supporting medical necessity.”
In plain English: there’s no proof that the test or follow-up visit was needed.
If your note says “routine follow-up” or “check cholesterol,” expect denials.
How to Prevent It:
- Document lab results (LDL, HDL, triglycerides) every time you assess or adjust therapy.
- Note medication response or non-compliance.
Mention medical decision-making:
“LDL remains elevated at 170 mg/dL despite statin therapy; plan to increase dose.”
That one sentence proves the necessity for both the visit and the test.
If labs were ordered but have not yet resulted, note that clearly:
“Follow-up for lipid results pending.”
Not Coding the Underlying Condition (Secondary Hyperlipidemia)
If hyperlipidemia is secondary to another disease (such as diabetes, hypothyroidism, or a kidney disorder), payers expect to see both codes — the primary condition and the hyperlipidemia.
If you only submit E78.2 or E78.5, it looks incomplete.
How to Prevent It:
Always code the underlying cause first.
- E11.69 → Type 2 diabetes with other specified complication
- E78.5 → Hyperlipidemia, unspecified
Correct sequence:
E11.69 (primary) + E78.5 (secondary)
Add a note in documentation:
“Hyperlipidemia secondary to Type 2 diabetes.”
This not only supports the diagnosis but also improves HCC risk scoring, which increases payer reimbursement in value-based programs.
Frequency Limitations or Screening Rules
Medicare and most commercial insurers set strict frequency limits for lipid testing.
For example:
- Medicare: Lipid screening only once every 5 years for asymptomatic adults.
- Aetna, Cigna, United: Usually allow one per year, unless a diagnostic need is documented.
If your claim shows “screening” without a supporting chronic condition or abnormal prior result, it may bounce back as:
“Frequency exceeded / not medically necessary.”
How to Prevent It:
Know payer frequency limits. Check payer portals or use eligibility tools like Availity or Change Healthcare.
Use the correct ICD-10 Z-code for screening:
- Z13.220 → Encounter for screening for lipoid disorders
Use E78.x codes for diagnostic testing.
Example:
- Annual screening: Z13.220 + CPT 80061
- Diagnostic recheck for mixed hyperlipidemia: E78.2 + CPT 80061
If you’re doing both in the same year, document:
“Diagnostic recheck due to abnormal lipid profile.”
Missing Modifiers for Same-Day Services
Sometimes lipid testing and evaluation are done on the same day.
Example: You bill 99213 (office visit) and 80061 (lipid panel) together.
Without modifier 25, the payer may assume the visit was routine and deny it as “included in lab service.”
How to Prevent It:
- Always add modifier 25 to the E/M code (99213–99215) when you perform both on the same day.
- Documentation must show separate and significant work beyond the lab order:
“Reviewed results, discussed lifestyle modifications, and adjusted medication.”
Correct billing example:
99213-25 + 80061 + E78.2
Diagnosis Code Doesn’t Match Plan Policy
Each payer defines “covered” diagnoses differently. Some may not cover E78.5 or E78.9 unless tied to comorbidities.
If you use a non-covered ICD-10 code for lipid testing, the claim may return as:
“Non-covered diagnosis per payer policy.”
How to Prevent It:
- Check the payer’s LCD (Local Coverage Determination) or medical policy for lipid disorders.
- Use covered codes (like E78.2, E78.00, or E78.01).
- If the test is truly for screening, use Z13.220 and bill under preventive benefits.
- Keep payer-specific cheat sheets handy at your billing desk.
Duplicate or Cloned Documentation
Some providers use template notes that repeat the same lipid information visit after visit.
Auditors can easily flag this as “cloned documentation,” leading to downcoding or post-payment recoupments.
How to Prevent It:
- Update every visit note with the current lipid results, any medication changes, and the patient’s response.
- Avoid copy-pasting entire sections.
- Even small updates like “LDL decreased from 190 → 160 mg/dL” show active management.
Not Linking Diagnosis to Lifestyle Counseling
If you provide lifestyle or diet counseling (CPT 99401–99404) but fail to link it to a lipid disorder, the claim gets denied as “no qualifying diagnosis.”
How to Prevent It:
Use E78.x or Z71.3 (dietary counseling) as secondary codes.
Example:
CPT: 99402 (Preventive counseling)
ICD-10: E78.2 + Z71.3
Final Thoughts
Hyperlipidemia may sound like a “routine” diagnosis, but in medical billing, it’s anything but routine. Every minor detail — from documenting lipid levels to choosing between E78.2 and E78.5 — can make or break your reimbursement.
The trick isn’t just coding correctly. It’s connecting the dots between clinical accuracy, payer rules, and precise documentation. When those three align, denials drop, reimbursements rise, and your billing process runs as smoothly as a well-oiled machine.
Here’s the takeaway:
- Be specific.
- Document every lab value and treatment reason.
- Link CPTs properly.
- Don’t rely on “unspecified” codes as shortcuts.
Let’s Make Your Hyperlipidemia Claims Effortless with Swiftcare
If you treat hyperlipidemia often — and most internal medicine or primary care clinics do — your revenue cycle depends on mastering these details. One coding slip might not hurt, but over hundreds of claims a month, it can quietly drain thousands of dollars.
At Swiftcare Billing, we live and breathe accuracy. Our team of certified coders and billing experts handles every detail — from verifying coverage and picking the correct ICD-10 code to appealing denials and tracking reimbursements until the last dollar hits your account.
We don’t just process claims. We prevent problems before they start.
Whether you run a solo practice or a multi-specialty group, our billing system is built to:
- Cut your denial rate by 30–40% within the first quarter.
- Increase clean claim submissions.
- Improve your cash flow consistency.
- Handle all payer types — Medicare, Medicaid, and commercial.
Schedule your free billing audit with Swiftcare today.


